Understanding Induction of Labor: What You Need to Know
Every expecting parent knows that pregnancy is an incredible journey, but sometimes circumstances arise that require medical intervention to ensure the health and well-being of both the mother and baby. One such intervention is the induction of labor. In this blog post, we will explore what a induction of labor entails, why it may be necessary, and how it is typically performed.
What is an Induction?
In short, it refers to the process of stimulating contractions before labor begins naturally. This procedure is usually recommended when there are health risks or concerns for either the mother or the baby. Each case is unique, and the decision for induction should be made by the pregnant mom herself, after seeking advice from her health care provider, evidence based information and weighing the benefits and risks of ALL of her options. Some inductions take hours, while most take 2-3 days, especially when the cervix isn’t soft & thin, ready for labor. Which should also be taken into consideration prior to agreeing to a medical induction of labor.
Why an Induction May Be Necessary?
There are several reasons why a healthcare provider may recommend an induction. Some of these reasons include:
1. Prolonged pregnancy: If a pregnancy exceeds 42 weeks, induction may be recommended due to an increased risk of complications such as stillbirth.
2. Fetal health concerns: If there are signs of fetal distress, growth restriction, or abnormalities, inducing labor may be necessary to protect the baby's well-being.
3. Maternal health conditions: Certain maternal health conditions, such as preeclampsia, severe cholestasis of pregnancy, or a major placental abnormality, may require the initiation of labor to prevent further complications.
4. Water breaking without contractions: If the water breaks prematurely, but labor does not start naturally within a certain timeframe, induction may be necessary to reduce the risk of infection.
It’s important to note, you should know the evidence based recommendations for certain pregnancy conditions yourself, as some providers may be basing care recommendations on old information. Many providers get busy with caring for patients that they often lag on implementing up-to-date care practices. And what’s best for one mom and baby may not be what’s best for every mom and baby! So, remember that this is your birth, your baby and your body that will be dealing with the weight of effects from an induction, which should not be taken lightly. And you do have the legal rite to say NO.
How Does an Induction Start?
The process of inducing labor may vary depending on the individual circumstances. Common methods of induction include:
1. Membrane sweeping: This technique involves a healthcare provider gently sweeping their finger around the cervix to separate the amniotic sac from the uterine wall, which can stimulate contractions. This can be helpful to increase the production of a hormone called prostaglandins which can soften and efface (thin out) the cervix prior to induction. In some cases-when women are 3-5cm dilated, and the cervix is starting to thin out as well prior to labor starting- those women show an increased rate of the membrane sweep kick starting labor.
2. Medications: Synthetic hormones such as Pitocin, cytotec or misoprostol may be administered to hopefully mimic the body's natural labor process and initiate contractions. Some of these medications are cervical ripeners that just thin and soften the cervix first, often being used overnight. Then pitocin (man made oxytocin) can be used to increase contractions to kick start active labor.
3. Rupturing the membranes: A healthcare provider may break the amniotic sac manually to encourage the onset of labor, especially if the mother is at least 3-5cm dilated and the baby’s head is super low and well engaged in the pelvis. In which case that’s often all the body needs to get going. This is typically done with a sterilized instrument and under controlled conditions. This is what we in the birth world call AROM (artificial rupture of membranes-water sack). For some expecting moms, this can be done once already in active labor (6cm+ with active contractions) to augment labor.
4. Combination of methods: Depending on the situation, a combination of methods may be used to induce labor effectively. This decision should be made by the laboring mother with the advice of her healthcare team based on the individual's needs.
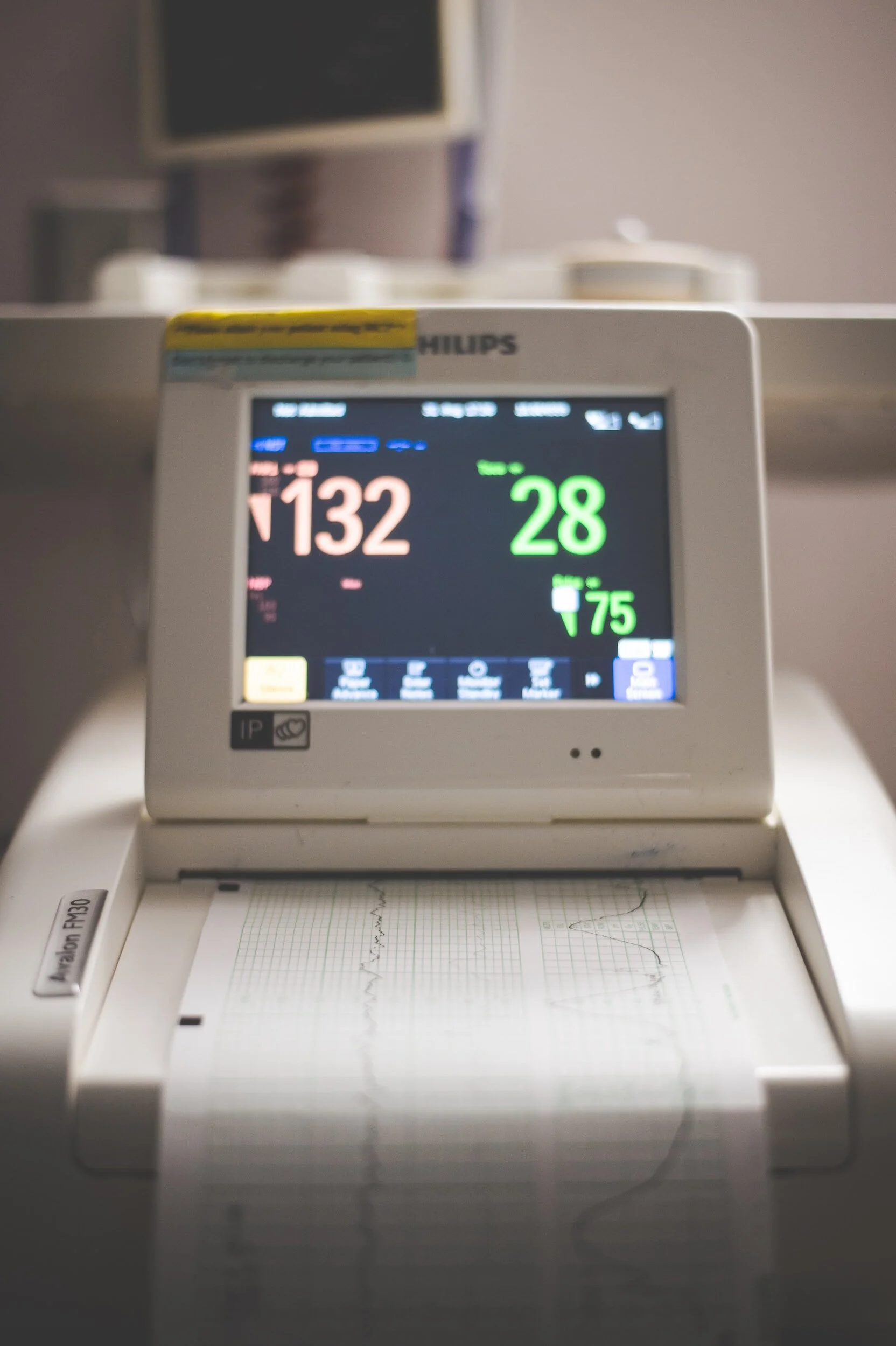
Photo by: Beloved Bits Boudoir Photography
Are There Risks to Inducing labor?
While sometimes birthing sooner rather than later can be the best thing for mom and baby, medical inductions are NOT to be walked into thinking there are no risks. There is MUCH risk to mom and baby when inducing. Some common risks associated with different methods of induction are:
Risk of hyperstimulation of the uterus- Where the uterus contracts too hard for too long- often resulting in baby not tolerating labor well. In turn causing the need for further intervention, and/or a cesarean birth.
Risk of infection- During an induction cervical exams are more frequent and more prevalently used as a way to assess if the induction methods are working to change your cervix and further the progress of birth. As a result antibiotics and birthing ASAP are recommended, often leading to further need for intervention, or cesarean birth.
Risk of pain level being increased- Often pregnant women experience a higher level of pain and discomfort when inducing labor as the result of trying to push the body to do something it’s not fully prepared to do. Which can lead to more frequent use of medical pain relief, which also comes with it’s own set of risks, i.e. stalling labor progress, dropping your blood pressure which can drop baby’s heart rate, limiting movement during labor which is important to facilitate progress, and possibly lead to a cesarean birth.
Risk of it NOT working- While many inductions do indeed dilate the cervix and bring baby down and out and into your arms, some inductions do NOT kick start you into labor. Often resulting in a “stall of labor” being defined and furthering the need for a cesarean birth.
While a cesarean birth isn’t the worst thing, it is major abdominal surgery that comes with it’s own risks, which can be life threatening for mom and shouldn’t be taken lightly.
During the induction process, the pregnant mom will often be asked to be continually monitored to ensure that both mother and baby are tolerating the labor well. This can allow healthcare providers to intervene if necessary and ensure a safe and healthy birth, as inductions come with MUCH risk to mother and baby. As does each of the options for induction. See Evidence Based Birth for more information on risks & benefits concerning inductions and be on the lookout next month for our upcoming in depth blog on the topic.
Conclusion
To get induced, is a medical intervention that you may determine is necessary, to protect the health and well-being of both yourself and your baby. By understanding the reasons behind induction, the various methods used, benefits and risks of the induction as well as waiting for labor to start on it’s own….. families can approach this process with knowledge and confidence. It is important to remember that the decision to induce labor should be made by the birthing woman, and done so on an individual basis after careful consideration of the risks and benefits of all the options available. If you have any concerns or questions about induction, it is always best to consult with your healthcare provider. And contact us today for more information on how you can prepare for your upcoming birth experience!